General
Who do the recommendations apply to?
The recommendations apply to everyone working or visiting in a hospital setting.
The use of a surgical face mask applies for all staff when not in patient-facing clinical settings (where appropriate personal protective equipment (PPE) should be used in line with published guidance), including:
- clinical (medical, nursing, allied health, diagnostics etc) and
- non-clinical staff (administration, porters, volunteers, cleaning, estates staff, contactors working on NHS sites, etc).
This guidance does not cover the use of masks for inpatients nor the use of masks as personal protective equipment. This should be managed in accordance with existing guidance.
What is the difference between a face mask and a face covering?
All surgical face masks are classified as either Type I, IR, II, IIR, and are medical devices provided by the hospital.
Face coverings can be cloth or homemade and should cover the nose and mouth of the wearer.
What supplies of face masks will be made available?
Surgical face masks will be made available through hospitals’ usual PPE deliveries. Since Sunday, 7 June 2020 a larger quantity of surgical masks have been sent out each day to help hospitals prepare for the additional need. Initially extra deliveries have focused on type IIR masks, and type Is and IIs will also be delivered and will be clearly labelled so staff do not use these in clinical settings.
Staff
Why is a recommendation now being made for all hospital staff to wear a surgical face mask (Type I or II) in non-clinical and social areas?
The recommendations have been made for all staff to help prevent the spread of infection. Evidence has shown that those infected with COVID-19 can have very mild or no respiratory symptoms (asymptomatic) and potentially transmit the virus to others without being aware of it, so it is important we take steps to reduce the risk of transmission from staff who may be asymptomatic.
A face mask worn in this context will help to reduce the risk of directly transmitting SARS-CoV-2 from the wearer to others and indirectly transmitting the virus to others from contaminated environmental surfaces.
What do the different surgical face mask types mean?
All surgical/medical face masks are classified as Type I, IR, II, IIR, and are medical devices. These are tested against BS EN 14683:2019. The tests check the bacterial filtration of the mask, the breathing resistance and the splash resistance. Type IR and Type IIR have an extra layer of material that ensures splash resistance and are not required for this purpose (but could be used in place of Type I or II masks as needed). Face coverings are not considered acceptable substitutes for staff.
Why are there different characteristic of surgical face masks?
- Manufacturers produced surgical masks in a variety of colours and the external layer can be white, green, blue.
- Masks can have ear loops or head ties to secure in place.
- The masks can be made of 2, 3 or 4 layers of material.
NB: All surgical masks have external pleats/vents, and these should always be worn downwards to the outside with the nose mould used to seal the material securely around the face.
Surgical face masks should cover both nose and mouth; not be allowed to dangle around the neck; not be touched once put on – only handle by the straps when putting on and taking off; and be changed when they become moist or damaged.
Do I need to wear a mask if I work in a private workspace where I work alone?
No, if you are working alone you will not be expected to wear a mask but when you leave the private work area to move through the hospital building, e.g. on an errand, or for meal breaks, you should put on a surgical face mask (Type I or II).
If you share an office with others, hospitals can perform specific (e.g. office or laboratory) workplace assessments. If these demonstrate robust and reliable COVID-19 prevention measures, including but not necessarily limited to social/physical distancing, hand hygiene and frequent surface and equipment decontamination, then face masks for staff may not be needed. All risk assessments that conclude that areas are COVID-secure should be documented.
What if I am already wearing a face mask for sessional use, do I need to change my mask?
Yes, if you are leaving a clinical area. This is because you have been wearing a mask to protect yourself when providing direct patient care. This should be removed when you leave the clinical area; and hand hygiene performed, prior to putting on a Type l or Type ll face mask.
What happens when I go to the hospital restaurant/staff room wearing my face mask?
You should continue to maintain social/physical distancing measures while in hospital restaurants or staff rooms. If eating/drinking, you should remove your mask and dispose as offensive waste. Do not place the face mask on dining tables or nearby surfaces. Once you have finished eating/drinking you should put on a new face mask to return to your clinical area or workplace. Secure supplies of face masks and alcohol hand rub should be made available in staff canteen areas.
At the end of the shift/day you should dispose of the face mask: you may use more than one mask depending on the duration of your shift.
How will staff have access to face masks when they arrive for work?
A supply of masks should be made available to staff as they arrive on the premises as near to staff entrances as possible (eg held at staffed reception desks). Handwashing or alcohol hand rubs should be available prior to donning (putting on). These area(s) should be large enough to accommodate several staff members to ensure physical distancing is maintained.
If, for example, staff are on-call and are required to work at various times, then they should be given a mask prior to leaving work.
Each organisation will need to identify a safe and secure method of supply. Face masks must be stored in accordance with manufacturers’ guidance.
How do I dispose of my face mask after work?
Each organisation will need to provide offensive waste bins and alcohol hand rub at facility exits to ensure that staff are able to remove masks and dispose of them and decontaminate their hands.
Will wearing a face mask in a non-clinical area protect me from getting
COVID-19?
The purpose of wearing a face mask in non-clinical areas is to prevent transmission from asymptomatic staff to others who they may come into contact with.
Symptomatic staff should be excluded from work.
Wearing a face mask is only one infection prevention and control measure that can help to limit the spread of COVID-19. Other measures include: compliance with social/physical distancing (two metres); frequent environmental cleaning; hand and respiratory hygiene.
What if I have a long-term health problem/breathing difficulties/claustrophobia and worry wearing a mask may make it worse?
Please discuss this with your line manager and occupational health department who will provide individual advice.
I work in an elective area (non-COVID) – do I need to wear a surgical face mask?
This recommendation is for all staff in all settings and areas of the hospital when not otherwise required to use personal protective equipment as per existing IPC guidance.
What does this mean for pregnant women during appointments and labour?
As inpatients, women in labour are managed under different guidance. Women in hospital setting as outpatients to antenatal or postnatal appointments will need to wear a face covering under the guidance. Children and babies under three years should not wear a covering, as per recently updated DHSC guidance.
How do I put on and take off my mask?
Local infection prevention and control teams can support training for staff who are not used to routinely wearing a face mask.
Outpatients and visitors
Why are we asking visitors/patients visiting the site to wear face coverings?
Outpatients or visitors coming to the hospital will need to wear face coverings to reduce the risk of transmitting coronavirus to others. Evidence has shown that those infected with COVID-19 can have very mild or no respiratory symptoms (asymptomatic) and potentially transmit the virus to others without being aware of it
Outpatients should be advised of the need to bring a face covering ahead of coming to hospital for planned and outpatient care (outpatient appointments etc); for example in appointment setting calls and confirmation letters.
What happens if an outpatient/visitor does not have a face covering when they come to the hospital?
If an outpatient or visitor does not have a face covering when they come to hospital, one should be provided by staff on arrival.
Local implementation plans should identify how this will be managed.
How do we communicate this new rule to visitors/outpatients?
The need for visitors/outpatients to wear a face covering when visiting the hospital site should be communicated through appointment letters, social media, local news stations/papers and through signage displayed at entrances to the site throughout wards and departments.
Staff should use any opportunity to inform patients of the rationale for face coverings. Consider using hospital volunteers to remind patients/visitors as they arrive on site. A face covering is not a medical/surgical mask. If outpatients and/or visitors do not have face coverings, the trust/hospital may need to provide surgical masks or consider having a stock of face coverings available.
A toolkit has been developed to support local communication with outpatients and visitors and will be made available to trust communications teams via regional communication channels.
What does this mean for shielding patients?
For those patients who are currently shielding, and who have been provided with a surgical face mask for their appointments, these should be worn. Where not already provided, patients should wear a face covering.
What about cloth/homemade/donated face masks?
Outpatient and visitor face coverings can be cloth and/or homemade (www.gov.uk/government/publications/how-to-wear-and-make-a-cloth-face-covering) All visitors will be expected to comply with two -metre social/physical distancing and the recommended hand hygiene measures.
Where applicable, visitors to high risk COVID-19 areas of the hospital or visitors of patients with confirmed COVID-19 must wear appropriate PPE as per the current IPC guidance.
Staff should comply with the guidance on wearing a surgical face mask (as appropriate when in clinical/non-clinical areas) while at work.
Does my face covering worn for religious beliefs/cultural practice qualify?
Face coverings worn as part of religious beliefs or cultural practice are acceptable, providing they are not loose and cover the mouth and nose.
What if an outpatient/visitor is unable to wear a face covering?
For some, wearing of a face covering may be difficult, and therefore all other measures must also be considered and introduced e.g. social/physical distancing, timed appointments; being seen immediately and not kept in waiting rooms. Individual risk assessments should be undertaken where required; for example, patients with mental health and learning disabilities. Such risk assessments must be documented.
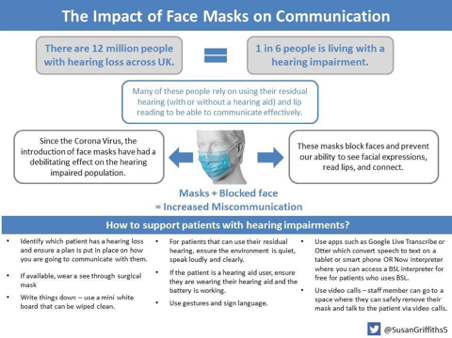
What about the impact of masks on communication for people who are deaf or have a hearing impairment?
The use of face masks due to the coronavirus pandemic may have an impact on patients who are deaf or have a hearing impairment as they can block the face of healthcare workers and prevent the ability to use visual cues such as facial expressions and lip reading.
The Government’s PPE procurement team has sourced an initially small number of clear surgical face masks to support communication with patients who may be deaf or hearing impaired. They are working with regions to identify where those are best distributed.
Where clear masks are not possible, the below diagram outlines some good communication tactics to consider supporting patients and visitors who are deaf or have a hearing impairment: