Guidance on the use of Non Invasive Ventilation (NIV) and High flow Oxygen (HFO (Airvo)) in the context of COVID-19 and severe ventilatory failure.
Aerosols generated by medical procedures are one route for the transmission of the COVID-19 virus. Both the use of NIV and HFO are considered aerosol generating procedures. Use of these modalities clearly has implications for infection control and outcome. NIV and HFO will generally not be used for patients who are COVID-19 positive.
NIV and HFO can be provided in the Respiratory Ward environment (2B/2C). Ward based NIV will continue to be provided to those patients where Critical Care is NOT appropriate and the ceiling of treatment will be NIV e.g. patients with Chronic Obstructive Pulmonary Disease or neuromuscular weakness..
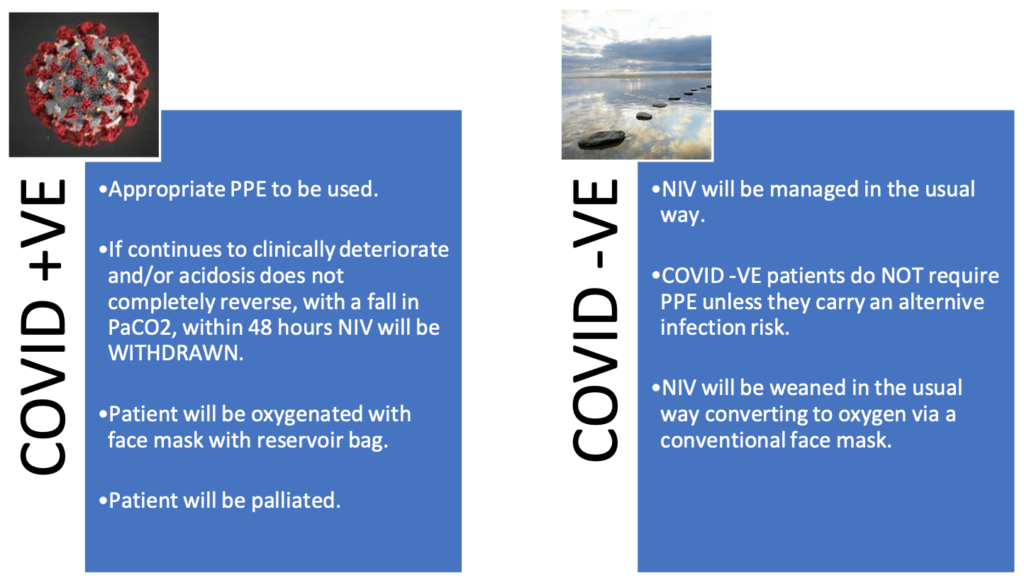
If a patient is negative they will continue to be treated with NIV as directed by the respiratory team.
NIV will NOT be initiated in any patient unless:
- Appropriate COVID-19 swabs have been taken.
- The ceiling of care of NIV is clearly documented.
- The CPR status of the patient is appropriately documented in the case notes.
Once COVID-19 swab result is available two pathways will emerge.
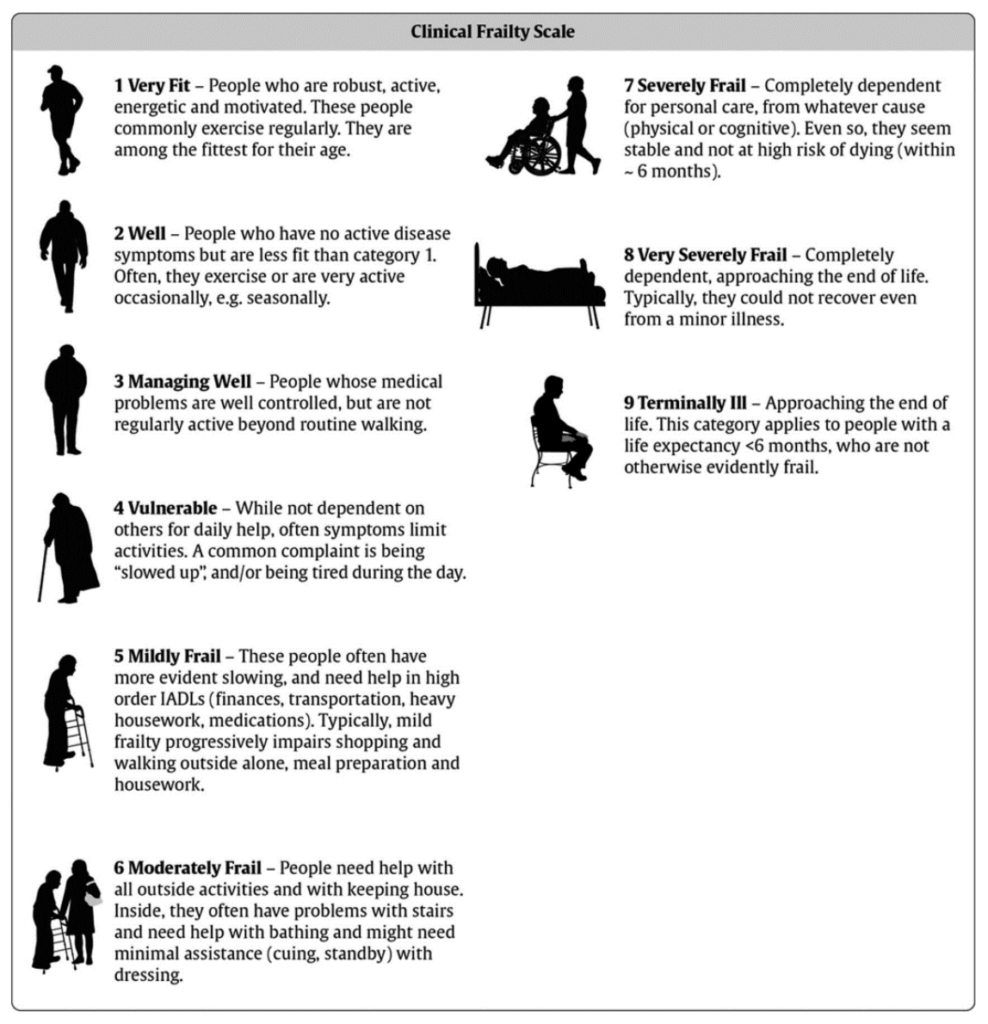
Overall management will be governed by performance status as measured by the CLINICAL FRAILTY SCALE and whether the patient is a candidate for critical care.
If a patient’s clinical frailty is deemed 5 or more they are less likely to benefit from organ support on Critical Care. A decision should be made by the treating team regarding the ceiling of treatment and this should be discussed with the patient (if possible)
Where decision making is difficult, support may be required from clinical colleagues.
If a patient is deemed not to be suitable for escalation to Critical Care, then this should be clearly documented in the case notes along with a treatment plan and a completed DNA-CPR (Lilac) Form.
If a patient’s clinical frailty is deemed 4 or less they may be considered a candidate for ITU. Critical care assessment should occur as quickly as practically possible.
In the event that the patient is unsuitable for critical care oxygen will be used (up to a maximum of 15 litres using a face mask with reservoir bag). Not for CPR status must be appropriately documented in the case note. Palliation as appropriate should be initiated.
**In the event that a patient is COVID-19 negative then HFO can be considered in suitable patients
Further considerations.
- Respiratory anticholinergic medications (Atrovent) should be used with caution in all patients that have suspected or confirmed COVID-19, who require oxygen.
- Saline nebs tds/NACSYS 600mg od should be considered in all patients that have suspected or confirmed COVID-19, who require oxygen.
- NSAIDS should be avoided.
- Patients who normally use home CPAP or NIV and are using their own machine whilst in hospital (either prior to COVID 19 testing or are confirmed COVID 19) must:
- Use an additional filter between the mask and exhaust port which should be changed every 24 hours.
- Remove any humidification setup – either integral or separate.
Any NIV/CPAP, including that used in ED, must only be provided in a side room with recommended PPE (for aerosol generating procedures) until such time that the patient is confirmed COVID negative.